당뇨병 환자에서 다발 소농양이 동반된 급성세균화농근염
Acute Bacterial Pyomyositis with Multiple Small Abscesses in a Diabetic Patient
Article information
Bacterial pyomyositis (PM) is a subacute bacterial infection of skeletal muscles predominantly caused by Staphylococcus aureus. It commonly presents as a solitary abscess in the quadriceps muscle [1,2]. While PM is frequently observed in tropical regions following a penetrating trauma, it has been increasingly reported in intravenous drug abusers, diabetics, malnourished individuals, and immunocompromised patients [1]. The rarity of PM and its nonspecific clinical presentation often contribute to delayed diagnosis and potential long-term disability [3]. We present a case of acute PM in a 59-year-old diabetic male showing multiple small abscesses in both thighs without a preceding trauma.
A 59-year-old male with diabetes mellitus (DM) and hypertension presented to the emergency room with gait disturbance and severe thigh pain. The patient had experienced general fatigue and myalgia for the past three days. On the fourth day, the severe myalgia in both thighs rendered the patient unable to walk. Prior to the onset of myalgia, the patient had stood for an extended period at a funeral. The patient had the following vital signs: a temperature of 38.1°C, a pulse of 91 beats per minute, a respiratory rate of 20, and a blood pressure of 120/77 mmHg. Initial laboratory findings revealed an elevated C-reactive protein (CRP) level of 18.18 mg/dL, a glycated hemoglobin level of 8.70%, and normal counts for leukocytes, creatine phosphokinase, and lactate dehydrogenase. Physical examination revealed severe tenderness upon palpation in both thighs. The patient denied any history of trauma, injection, or strenuous activities. Neurological examination showed proximal symmetric weakness of lower extremities (Medical Research Council grade IV). However, muscle strength could not be accurately assessed due to severe pain during the test. The patient was unable to stand or walk due to severe thigh pain. Computed tomography of the chest, abdomen, and pelvis ruled out any fever-inducing causes. Blood and sputum cultures were performed and the patient was empirically treated with ceftriaxone and clindamycin. Magnetic resonance imaging (MRI) revealed multiple small mass or cyst-like enhancing lesions combined with perilesional infiltrative enhancement distributed around intramuscular vascular branches in both thighs, with vastus muscles affected the most severely (Fig. 1A-D). Serological tests for autoimmune diseases, vasculitis, and infectious diseases including human immunodeficiency virus yielded negative results. Blood culture was positive for Staphylococcus aureus, leading to a modification in the antibiotic regimen based on results of antimicrobial susceptibility test. After two weeks of antibiotic treatment, his CRP decreased and normalized (Fig. 1E) and his symptoms completely resolved.
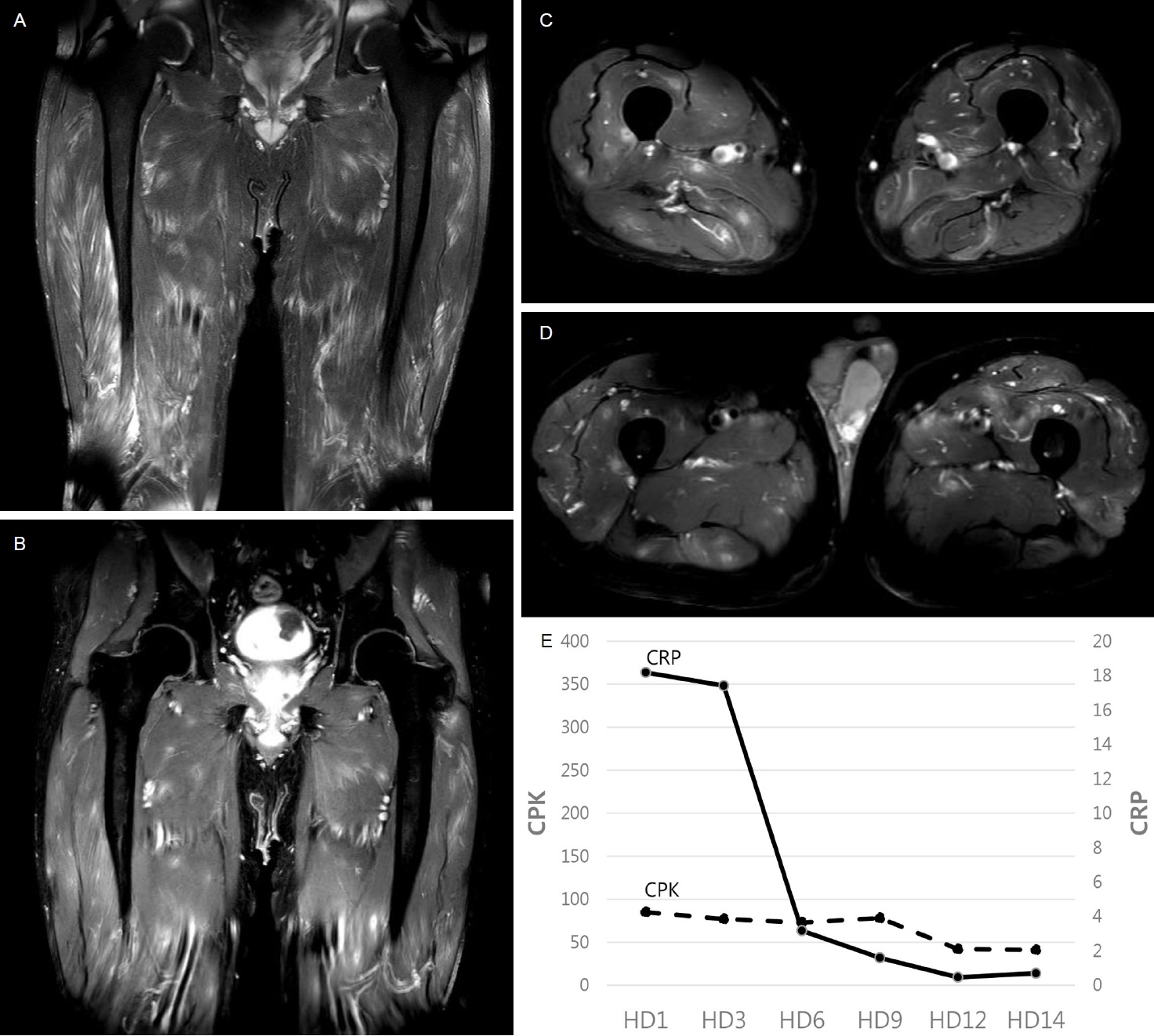
(A) Coronal T2-weighted turbo spin-echo fat-suppressed image showing multiple patchy hyperintense lesions, (B) Coronal and (C, D) axial postcontrast T1-weighted modified Dixon images revealing multiple enhancing lesions with perilesional infiltrative enhancement in both thighs. (E) Serial changes in serum CPK and CRP. CPK, creatine phosphokinase; CRP, C-reactive protein; HD, hospitalization day.
Most etiologies of myalgia can be divided into conditions causing diffuse or localized symptoms. Diffuse myalgia may arise from systemic rheumatic disease, fibromyalgia, infection, medication use, metabolic derangements, hypothyroidism, or psychiatric causes. Localized myalgia can be attributed to strenuous activity, soft tissue disease, PM, myofascial pain syndrome, muscle infarction, or compartment syndrome. The presence of fever raises suspicion for rheumatic disease or infection such as PM, endocarditis, viral infection, and impending sepsis. An accurate diagnosis requires a comprehensive approach, including a detailed medical history, thorough physical examination, and relevant laboratory tests to identify potential causes of myalgia and guide appropriate management [4].
Although the pathogenesis of PM remains unclear, transient bacteremia with minor trauma might be a contributing factor as PM often develops without an apparent penetrating injury [2,3]. Bacteremia alone is insufficient to cause PM as skeletal muscle tissue is resistant to bacterial infection. Alteration in local muscle tissue structure due to trauma can impart muscle susceptibility to bacterial implantation during a subsequent bacteremia episode [1,3]. In diabetic patients, basement membranes of striated muscle capillaries are markedly thickened, potentially leading to decreased diffusion of oxygen, glucose, and insulin into skeletal muscle tissues [5]. These factors may increase susceptibility to infection, explaining why DM is the most frequently observed underlying disease in PM cases [2]. In the present case, DM and muscle fatigue resulting from prolonged standing might have contributed to the development of PM.
PM can affect any muscles in the body, although it typically involves a single muscle, often the largest muscle in the pelvic girdle or lower extremities. However, in 11% to 43% of patients, multiple muscles can be affected [3]. MRI plays a crucial role in timely diagnosis of muscle infection. Pus within the abscess can appear hypointense, isointense, or hyperintense on T1-weighted images depending on the proteinaceous content of fluid collection [1]. In our case, MRI findings indicated a potential of vasculitic myopathy or inflammatory myositis. However, positive blood culture result and subsequent complete resolution of myalgia following appropriate antibiotic treatment provided substantial support for the presence of multiple small abscesses caused by S. aureus bacteremia.
Regardless of the underlying etiology, PM progresses through three distinct stages: an invasive stage characterized by diffuse inflammation, a purulent stage marked by focal abscess formation, and a late stage associated with septic state [2,3]. Its onset is insidious, with edema and pain in the involved muscle. Patients usually become aware of their illness during the purulent stage of PM [2].
A prompt and accurate diagnosis of PM is crucial for effective management and prevention of life-threatening complications. Therefore, a high level of suspicion is necessary to diagnose PM as early as possible in diabetic patients who experience acute buttock or thigh myalgia following activities that might lead to muscle fatigue.
Notes
All authors have no conflicts of interest.