Sensory Guillain-Barr├® syndrome (GBS) is an acute, monophasic neuropathy characterized by sensory disturbance without motor involvement [1-3]. Acute neuropathies presenting with sensory symptoms and signs have been described as sensory GBS, acute sensory ataxic neuropathy (ASAN), ataxic GBS, acute ataxic neuropathy [1,4-6]. This condition remains very rare to date so a timely and accurate diagnosis is important [1,4-6]. Because of the scarcity and heterogeneity of sensory GBS and similar cases, and the lack of adequate definition, the relationships between these conditions are controversial, and the terminology is often confusing. [1-4,6]. This makes clinicians challenged to diagnose and delay giving a proper treatment to a patient [1-5]. Sensory GBS patients show heterogeneous sensory symptoms like paresthesia, pain, hypesthesia, ataxia with hypo- or areflexia [1-4,6]. It means sensory GBS can involve large myelinated fiber, resulting in ataxia, loss of touch, vibratory perception and also can involve small and medium-sized fiber, causing pain and tingling, burning allodynia [1,4,5]. It can be also accompanied by autonomic symptoms presenting with orthostatic hypotension, syncope, abdominal pain, nausea, vomiting, or diarrhea [1,2,5]. And like other GBS, albumino-cytologic dissociation is observed, but normal cerebrospinal fluid (CSF) finding also can be observed [1,4,5]. On serologic test, anti-GQ1b immunoglobulin (Ig) G, anti-GD1b IgG have been identified in sensory GBS [1,4]. The electrophysiologic findings in sensory GBS include sensory nerve conduction slowing or decreased sensory nerve action potential, but the findings are often normal in the early stage, and usually normal motor nerve conduction study [1-6]. Owing to this clinical and pathological diversity, accurate characterization and classification of sensory GBS are needed [1,4]. Herein, we report an autonomic symptoms dominant sensory GBS in a patient with systemic lupus erythematosus (SLE).
Case
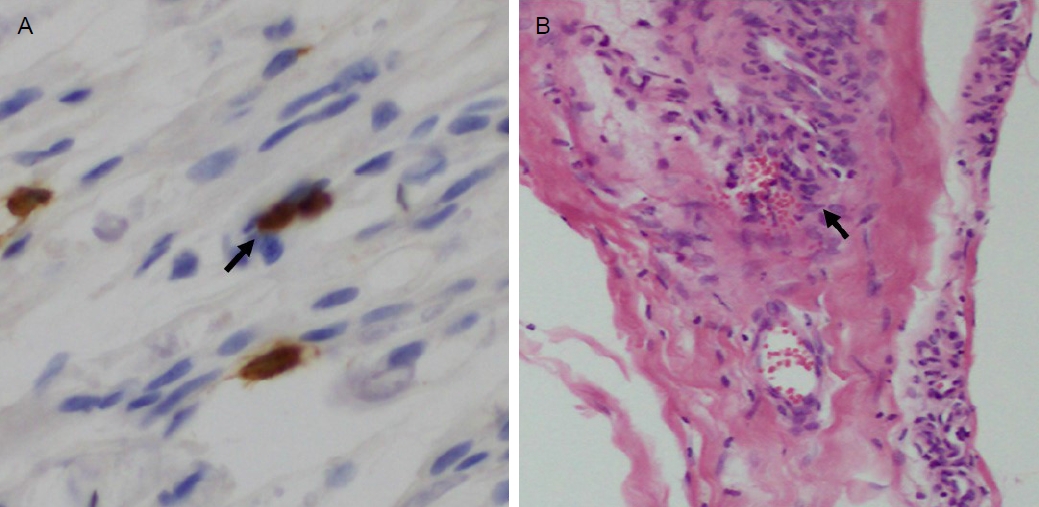
A 33-year-old woman with an underlying SLE complained of orthostatic dizziness and syncope, persisting for ten days. She also reported diarrhea, nausea, vomiting, and pain in the abdominal area and all extremities. She has been controlled with oral prednisolone (5 mg/day) and denied a family history of neurological disease. On neurologic examination, she had hypesthesia to pain and temperature on her face and trunk without sensory level, and position and vibration on extremities. She also showed decreased deep tendon reflex, dysmetria, dysdiadochokinesia, and decomposition on both side extremities with intact muscle power. We could not examine her gait and posture because of her orthostatic syncope. Blood pressure in the supine position was 110/70 but decreased to 80/60 in sitting position. Brain magnetic resonance imaging revealed unremarkable findings including the cerebellum. Although the motor nerve conduction study and electromyography showed normal findings, the sensory nerve conduction study showed decreased nerve action potentials without decreased conduction velocity, suggesting axonal sensory polyneuropathy (Table 1). The laboratory tests revealed positive anti-GM1 IgG and anti-GD1 IgG antibodies. Chest and abdomen computed tomography scans and other laboratory studies, including CSF analysis, paraneoplastic antibodies, autoimmune antibodies, and porphyrin were normal. While undergoing diagnostic procedures, to prevent delay of treatment considering lupus vasculitis and sensory neuronopathy associated with SLE, the patient received two cycles of intravenous high-dose methylprednisolone treatment (62.5 mg/day) for five days. However, her symptoms were not resolved. Subsequently, we conducted a sural nerve biopsy to distinguish vasculitis related to SLE. The sural nerve biopsy showed increased myelin destruction with T-cell infiltration without evidence of vasculitis (Fig. 1) [5,7]. Together with these clinicopathologic and laboratory findings, we diagnosed her with sensory GBS. We administered two cycles of intravenous immunoglobulin (0.4 mg/kg/day) for 5 days, and neurologic and clinical symptoms were significantly improved.
Discussion
We present a case of sensory GBS which was presented with autonomic and ataxic neuropathy with acute progression. Although the CSF finding was normal, considering the nerve conduction study and electromyography results suggesting axonal sensory neuropathy, the presence of anti-GD1 IgG antibody, and the sural nerve biopsy findings, the diagnosis was compatible with sensory GBS. Moreover, we could exclude lupus vasculitis and sensory neuronopathy associated with SLE since the disease activity was stable and high-dose of steroid was ineffective. More specifically, considering the previous case report and literature about sensory GBS and related cases, this patient could be diagnosed with ASAN or acute sensory and autonomic neuropathy which can be accompanied by dysautonomic symptoms [1,2,4,5]. And although patient presented with only profound dysautonomic symptoms like our case, clinicians should consider sensory GBS with detailed history taking, neurological examinations and various diagnostic tools.
Because of the scarcity and heterogeneity of sensory GBS, to resolve the uncertainty of definition, classification, and terminology, there was an attempt to establish a systematization based on the possible site of primary damage [1,4]. The differences of antibody attacking sites may explain the differences in clinicopathological and electrophysiological features. Uncini and Yuki [1] classified cases into three subtypes including acute sensory demyelinating polyneuropathy, acute sensory large-fiber axonopathy-ganglionopathy, and acute sensory small-fiber neuropathy-ganglionopathy. The clinical and electrophysiological features of our case are most likely between acute sensory large-fiber axonopathy-ganglionopathy and acute sensory small-fiber neuropathy-ganglionopathy.
Considering GBS can have a poor prognosis, rapid diagnosis and proper treatment are important. Prompt and accurate diagnosis of sensory GBS patients with diverse diagnostic methods is needed. Early treatment with intravenous immunoglobulin treatment could be successful for those patients.
Sensory GBS is unclear era because there are no established diagnostic criteria, classification, and terminology. Although there has been small number of cases and they have shown different clinical presentations and electrophysiological findings, to establish diagnostic criteria and classification, further studies combining data from current and previous reports and studies on sensory GBS are needed. Although sensory GBS is a very rare entity in the GBS subtypes and sensory neuropathy, the possibility of sensory GBS should also be considered when a patient present with sensory symptoms.